SHARE WITH FRIENDS:
The disease occurs in all countries of the world. This disease can be accompanied by various clinical signs due to changes in the lymph nodes and reticuloendothelial system, and is similar to diseases such as leukemia, lymphogranulomatosis, sore throat. It therefore leads to diagnostic errors. In young children, the disease takes on a vague and mild form and is difficult to diagnose. Therefore, doctors must be fully informed about this disease.
EPIDEMIOLOGY.
The source of the disease is a sick person and a virus carrier. The washing path is through air-droplets. In some cases, it can be transmitted through contact, alimentary and transfusion routes. But in practice, these routes of transmission are rare. The susceptibility to the disease is very low. It is mainly noted in adolescents and middle-aged people. It is more common in the colder months. Infectious mononucleosis occurs sporadically. But it can also spread in groups (family, schools, military units). Acquired immunity, stable, no recurrence. Infectious mononucleosis is less common in infants and children under one year of age because immunity is transmitted to children through the transplants.
ETIOLOGY.
According to many scientists, the causative agent of infectious mononucleosis is the Epstein-Barr virus. The virus belongs to the family of DNA-storing herpes, has lymphoproliferative properties. The difference from other viruses is that it does not cause cytolysis and only multiplies in B-lymphocytes. The virus persists in cells for a long time and in some cases has the ability to reproduce again. However, the reasons for the detection of this virus in Berkitta lymphoma, nasopharyngeal carcinoma and lymphogranulomatosis, in addition to infectious mononucleosis, are still unclear.
PATHOGENESIS.
The pathogen enters the body through the mucous membranes of the mouth, throat and upper respiratory tract. Redness and swelling of the mucous membranes are observed at the site of entry of the pathogen. There are 5 stages in the pathogenesis of infectious mononucleosis: Stage I - the introduction of the pathogen; Stage II - the transfer of the virus through the lymphogenic pathway to the regional lymph nodes, their hyperplasia; Stage III - viremia and systemic reaction of lymphoid tissue; Stage IV - infectious-allergic condition; Stage V - the formation and recovery of immunity against this disease. The basis of pathological changes in infectious mononucleosis is the proliferation of elements of the macrophage system, diffuse or focal infiltration of tissue indeterminate mononuclear cells. In rare cases, histological examination reveals focal necrosis of the liver, spleen, kidneys.
CLINICS.
The incubation period has not been fully studied. According to scientists, it can last up to 5-21 days or up to 1 month. The disease often begins with a sudden rise in body temperature. However, typical clinical signs for infectious mononucleosis appear at the end of the first week of the disease.
Clinical signs of the initial period:
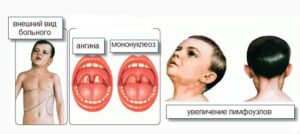
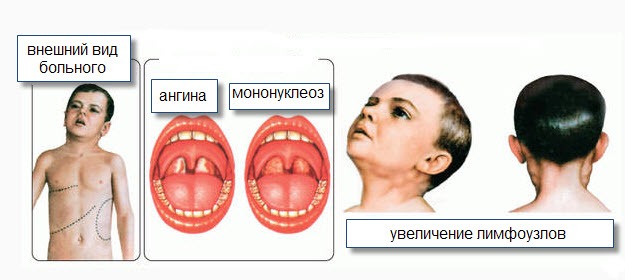
increase in body temperature, enlargement of the lymph nodes in the neck, inflammation of the tonsils, difficulty breathing through the nose.
An enlarged liver and spleen can be felt by the end of the first week and the beginning of the second week.
In the blood, indefinite mononuclear is formed. In some cases, the disease begins slowly.
In this case, the disease may be accompanied by a rise in body temperature for 2-5 days, weakness, slight catarrhal inflammation of the upper respiratory tract, in 1/3 of patients at the beginning of the disease body temperature is subfebrile or normal, by the end of the first week going up to 38-40 C.
Lymphadenopathy (viral lymphadenitis) is a persistent and primary symptom of the disease, first with enlarged lymph nodes located behind the ear, under the jaw, and at the back of the neck. Most often, lymphadenitis is bilateral, in some cases on the left side.

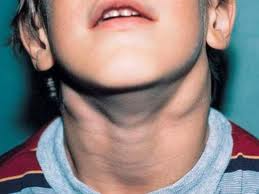
Chow, axillary lymphadenitis is less common. The size of the lymph nodes can range from a pea-shaped nut to a chicken egg. Stiff elastic when held, slightly painful and not attached to the surrounding tissue. The skin above the lymph nodes has not changed. In some cases, tumors may appear in the tissues around the lymph nodes. After 15-20 days, the lymph nodes return to normal. Lymph node abscess is rare in infectious mononucleosis.
Damage to the throat and larynx is considered a persistent and obvious clinical sign of infectious mononucleosis. First of all, damage to the tonsils is manifested by symptoms of various types of angina (catarrhal, follicular, lacunar, ulcerative and necrotic). Examination of the patient's throat reveals redness and swelling of the tonsils, tongue, back wall of the larynx. In some cases, almond glands develop coatings of various shapes. The coatings are whitish-yellow or gray in color, bumpy and easy to move.

Often the inflammatory process also spreads to the nasopharyngeal glands. They cause nasal congestion, ie flu symptoms, due to their enlargement. The patient's voice changes, breathing becomes difficult, and breathing through the mouth is observed.
Hepatosplenomegaly is detected in 97-99% of patients. Liver volume increases from the first day of illness and peaks by day 4-10. In some cases, liver function is also altered (jaundice in the skin and eyes, increased aminotransferases, thymol and sulema tests). The decrease in liver volume is gradual and can last up to 2-3 months. Enlargement of the spleen is also one of the main clinical signs of infectious mononucleosis. All patients who come to the hospital can be palpated with an enlarged spleen in the first three days. It reaches its peak in 4-10 days. The reduction and normalization of the volume of the spleen occurs earlier than that of the liver. This corresponds to the end of the 3rd week.
Changes in the blood. For infectious mononucleosis, a small amount of leukocytosis (15–30 x 10) is associated with an increase in ECHT of 20–30 mm / s. The most important changes are lymphocytosis, monocytosis, and the appearance of indeterminate mononuclear cells (10–70%) in the blood.
Some patients may not have clinical signs of infectious mononucleosis. With a gradual decrease in body temperature, the patient's general condition begins to improve and other clinical signs of the disease gradually disappear.
Clinical classification of infectious mononucleosis
1.Types
Exactly
Indefinite:
A) in the hidden position
B) without clinical signs
C) visceral
2. By weight
Light
Average weight
Heavy
DIAGNOSIS.
The main clinical signs are: fever, lesions of the throat and larynx, enlargement of lymph nodes, as well as hematological changes (increased ECHT, the presence of indeterminate mononuclear cells, lymphocytosis, leukocytosis). Uses various hemagglutination methods based on serological analysis. The simplest high-performance serological method is the equine erythrocyte attachment reaction (RA) in this instrument window. This reaction is positive in 99% or more of patients with infectious mononucleosis, while in other diseases it is almost always negative.
COMPARATIVE DIAGNOSIS. Infectious mononucleosis
Don't worry,
ORVI,
Viral hepatitis,
It is carried out with diseases such as lymphogranulomatosis.
COMPLICATIONS.
Rare. The most important are otitis, paratonsillitis, sinusitis, pneumonia. Rarely, rupture of the spleen, acute liver failure, acute hemolytic anemia, myocarditis, meningoencephalitis, neuritis, polyradiculoneuritis occur.
TREATMENT
There is no private cure. Mainly hyposensitization, marked and strength-enhancing treatment
methods are used (vitamins C, PP, B-group). If complications are observed, antibiotics are prescribed. Of course, gargling (iodine, furacillin solutions), hot compresses are recommended. In severe cases
glucocorticosteroids (1-1,5 mg / kg) are given.
PREVENTION.
There is no private prophylaxis. Hospitalization is based on clinical indications. Those in contact are not observed. Disinfection measures are not carried out. Quarantine will not be announced
© Doctor Muxtorov